
I lived with unexplained pain for years—fatigue, brain fog, joint and muscle pain. Every doctor I visited told me something different. Some blamed stress. Others ran tests that all came back “normal.”
After nine long years, I finally learned what was really going on: fibromyalgia. But the real problem wasn’t just the condition—it was how poorly it’s often diagnosed.
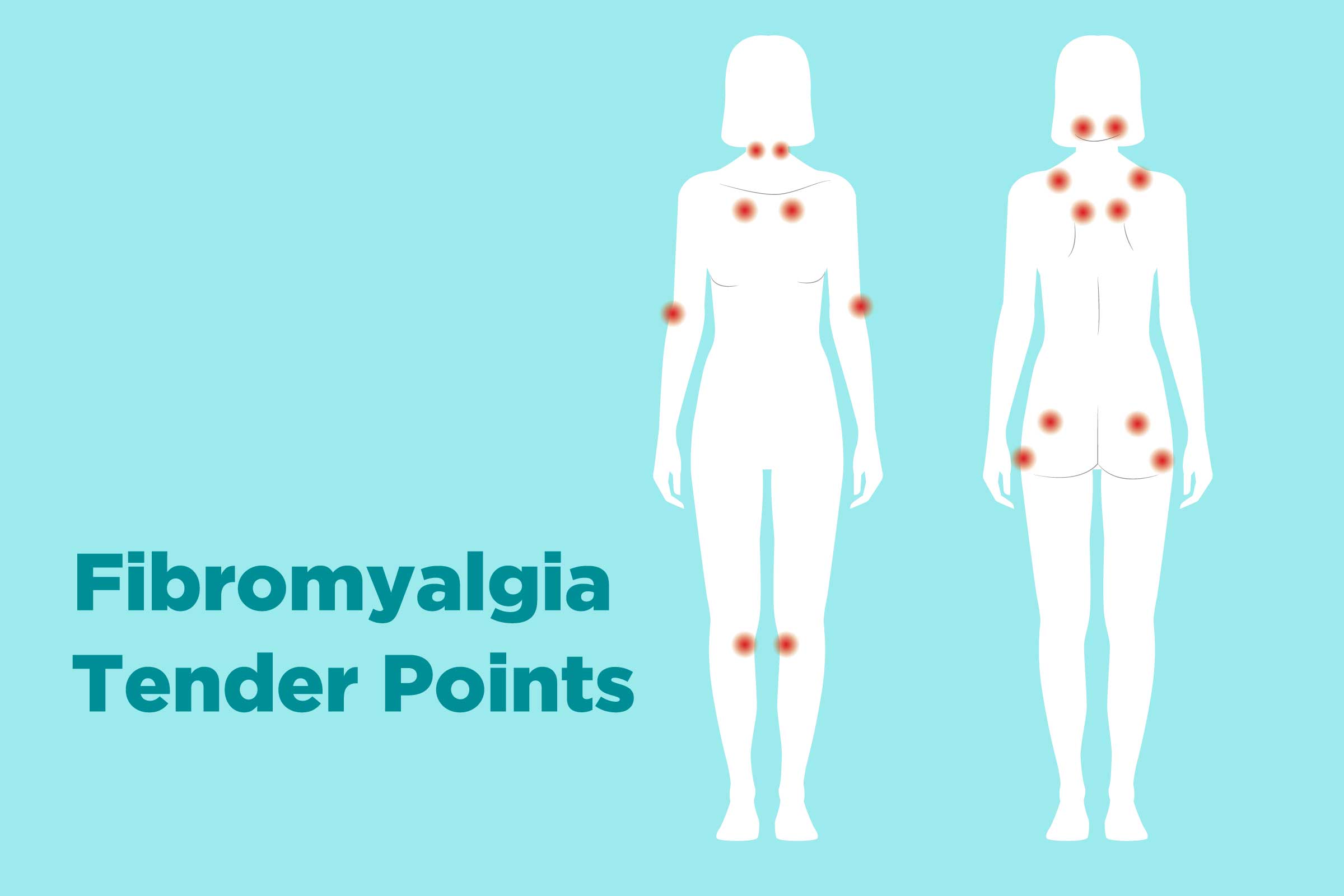
In the 1990s, doctors diagnosed fibromyalgia using a “tender point exam.” They’d press on 18 specific points across the body. If 11 or more hurt, and your pain had lasted over 3 months, you might get a diagnosis.
But this method had problems:
As a result, many people with real symptoms were told nothing was wrong.

In 2010, the diagnosis process changed. Doctors started using symptom checklists instead of pressing on points. They introduced two tools:
If symptoms had lasted 3 months or more and met scoring guidelines, a diagnosis could be made.
In 2016, the criteria improved again. Doctors now look for:
This made the diagnosis more accurate and more helpful for patients.

Even with better tools, fibromyalgia is often misunderstood or misdiagnosed. That’s because:
So if you’ve been struggling with pain and no one seems to get it—you are not alone.

We believe your story matters—and that diagnosis should reflect the whole person, not just a form.
Many of our clients came to us after years of confusion, doubt, and frustration. They’d seen multiple specialists, taken medications that didn’t help, and still didn’t know what was wrong.
At MAD, we take the time to listen, assess, and personalize every care plan.
Fibromyalgia is real. The pain is real. But so is the path to clarity. Let MAD help you find the answers you deserve—with a supportive, step-by-step approach made just for you.
How was fibromyalgia diagnosed before?
Doctors used a “tender point” exam—pressing on 18 spots to see if 11 hurt. This is no longer required.
What are WPI and SSS?
WPI tracks how many body parts hurt. SSS measures fatigue, brain fog, sleep quality, and other symptoms.
Why is fibromyalgia hard to diagnose?
Because symptoms overlap with other conditions and vary between people. It takes a full-body and full-history evaluation.
What makes MAD different?
We look beyond forms. We combine science, clinical tools, and compassion to truly understand your pain and create a custom care plan.
References
Wolfe F, Clauw DJ, Fitzcharles MA, et al. (2016). Revisions to the 2010/2011 Fibromyalgia Diagnostic Criteria. Seminars in Arthritis and Rheumatism, 46(3), 319–329.